COVID White Paper Series-06
 David Van der Vossen PE
David Van der Vossen PE
Senior VP of Engineering
LEED AP BD+C, CGD
As we continue our series on COVID-19 and preventable actions that we can put in place via building systems, let us take a deeper dive into the effect of humidity on transmission rates.
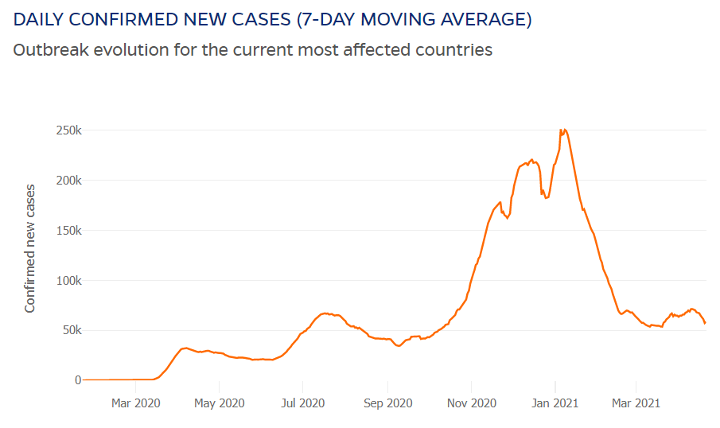
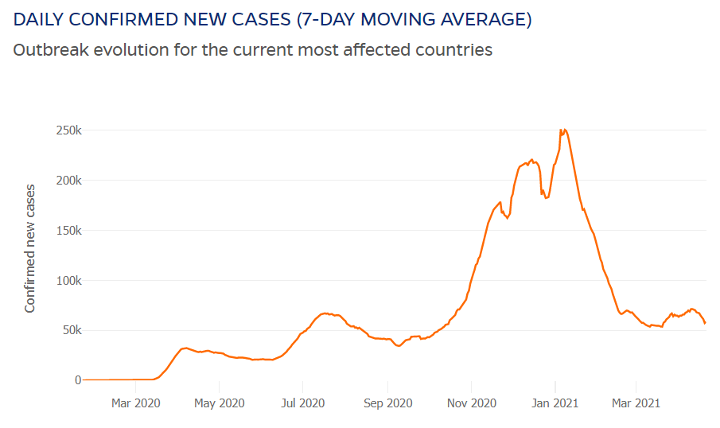
Hindsight is 20/20. Going into the winter, many experts predicted that we would see a significant uptick in COVID-19 cases. What did they know? Based on experience with other viruses such as the yearly flu, scientists knew that the combination of lower humidity and typical population patterns would most likely lead to an increase. Below is data from Johns Hopkins University that shows how this prediction played out between November 2020 and February 2021. As humidity levels decreased, COVID-19 cases did indeed grow.
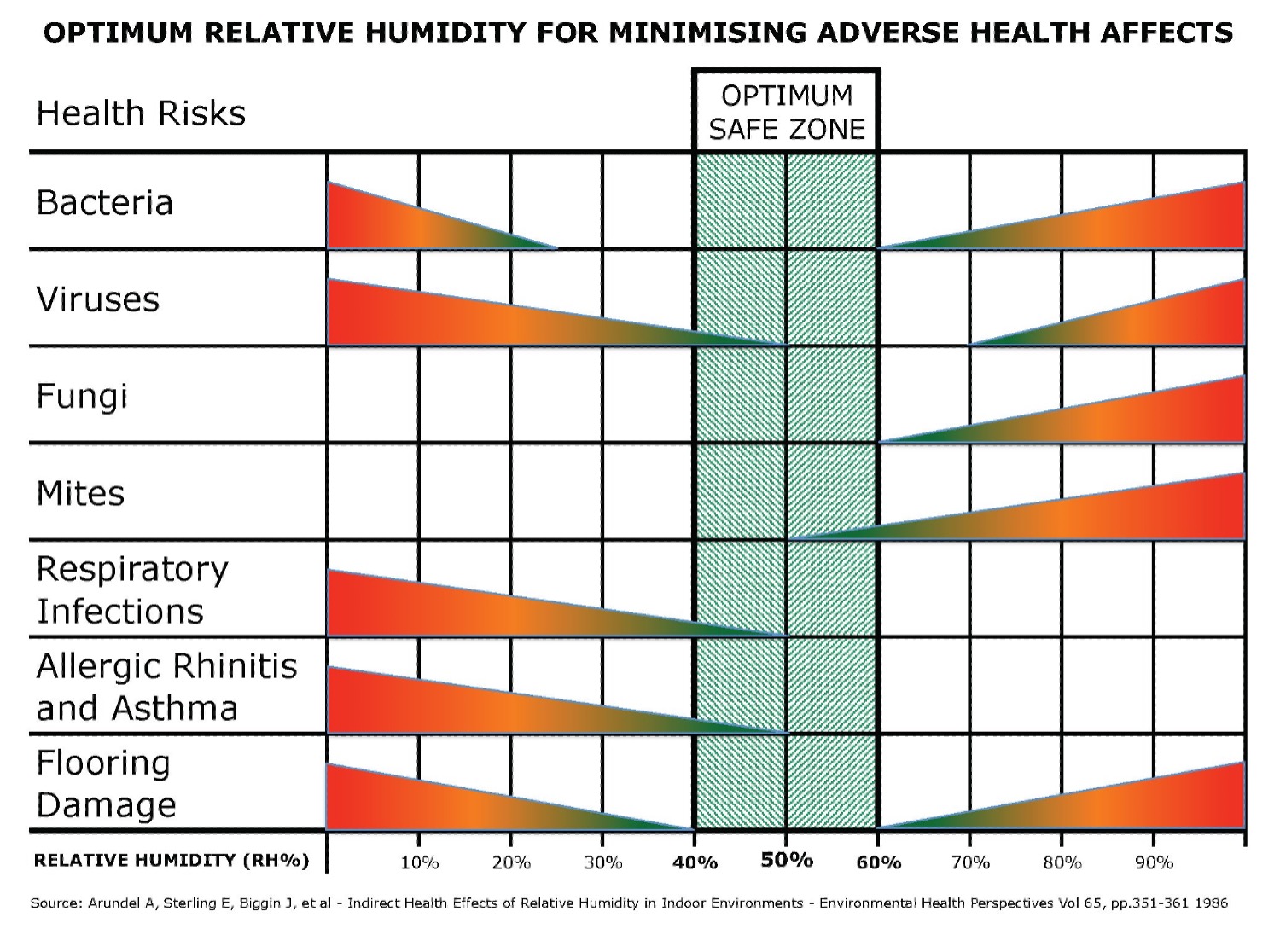
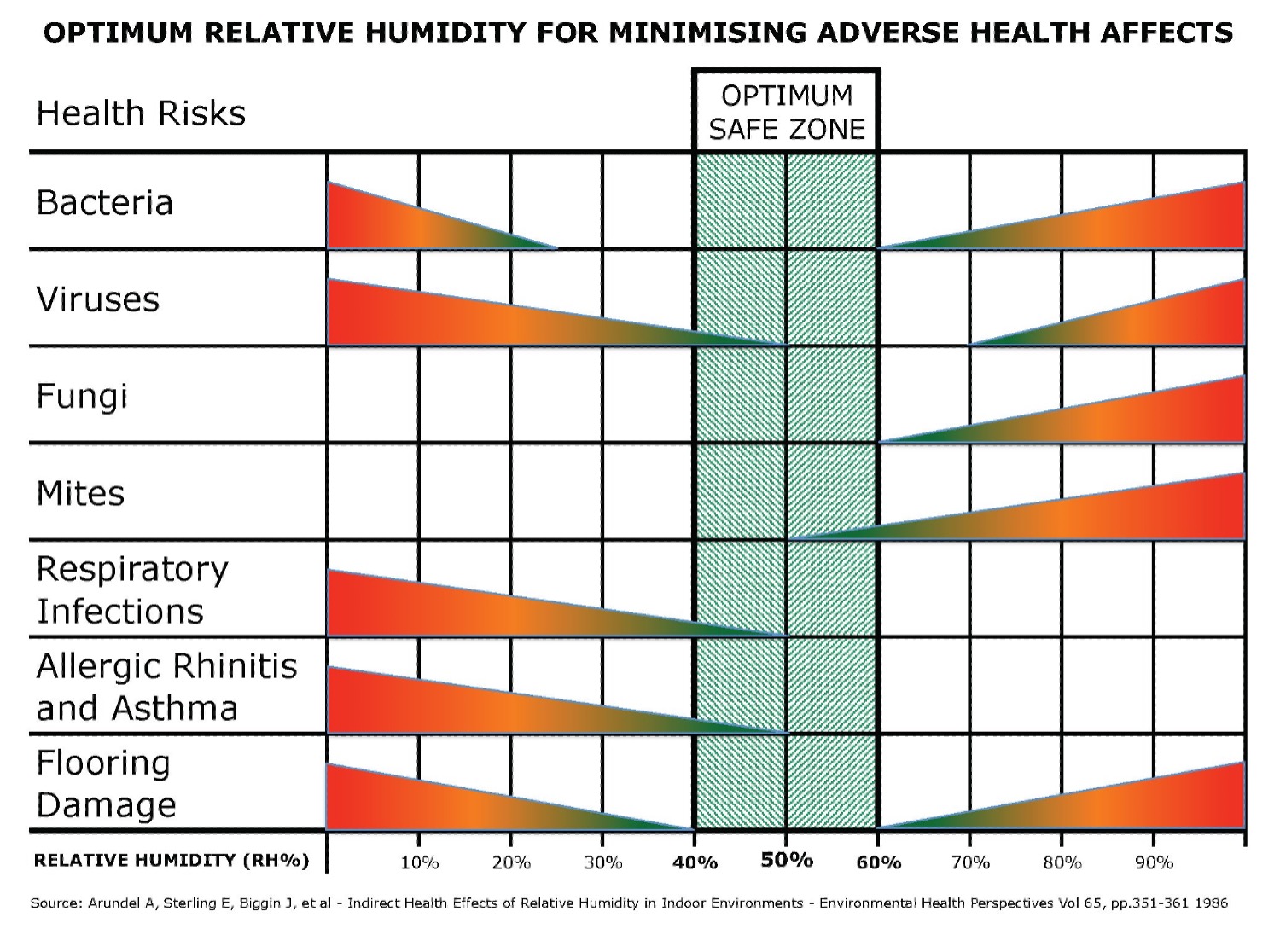
ASHRAE has long noted the indirect health effects of humidity based on humidity’s effect on viruses, bacteria, and other pathogens. Below is a chart demonstrating the optimal safe zone between 40-60% RH (relative humidity).
Looking specifically at viruses; what is happening relative to lower humidity in the winter months? Three concepts come into play which play a role in the increase in transmission rates: higher evaporation rates, increased time indoors, and lower ability to shed virus particles.
Increasing Evaporation Rates
As virus particles are exhaled, they are incased in water and mucus. If the water and mucus evaporate before the droplet encounters a surface, then the virus particle will remain airborne. This allows the particle to spread easily throughout the space as people then breathe them in.
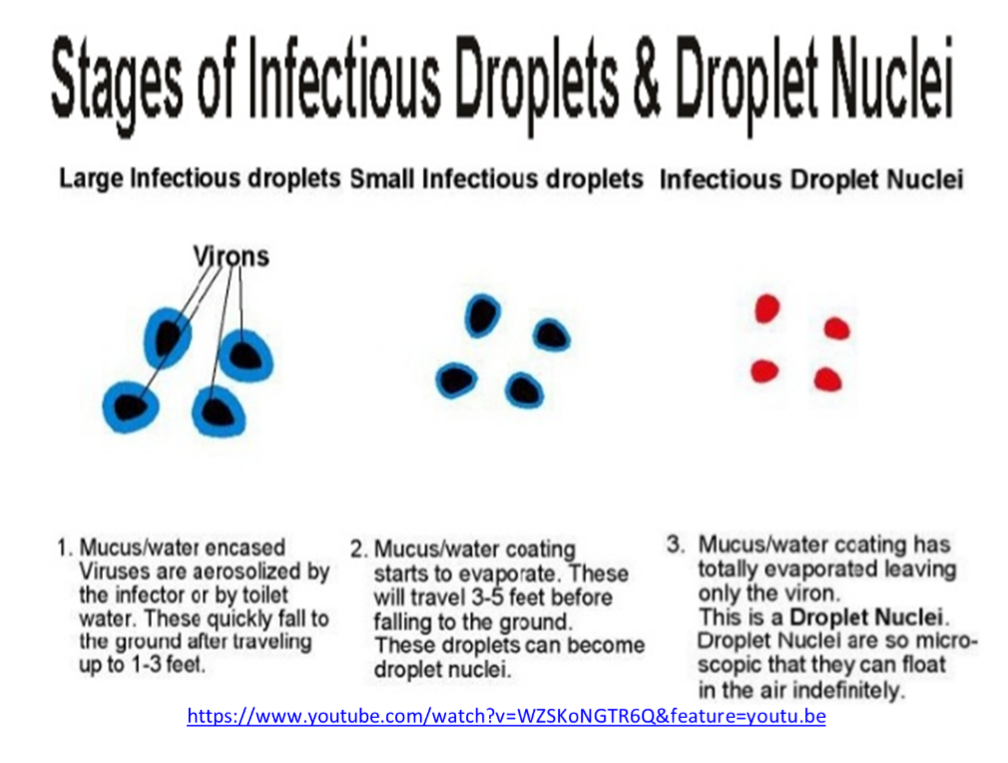
When humidity levels decrease, the number of virus particles that stay airborne rather than landing on a surface increase. During a 35-degree winter day, the indoor humidity of most homes and buildings will drop below 25% RH when no supplemental humidification system is present. This lower humidity significantly increases the number of droplets that evaporate and become aerosols. Thus, an increase in airborne concentration will increase the likelihood of people within the space breathing the virus in.
Time Indoors
In terms of aerosol transmission of viruses, exposure time and the aerosol concentration in a space are both significant players. The density of the virus particles in the air determines how many particles at any given time are ingested. How long someone stays within that environment also increases particle ingestion. Essentially, our exposure is equal to the rate of intake times the length of exposure. During the cold winter months, individuals inherently spend more time indoors, extending exposure time, and thus increasing transmission risk.
Exposure Risk
Breathing in a couple particles of COVID-19 will not give you the virus. To become infected, an individual needs to breathe in what is called an “infectious dose” level. The infectious dose level is a very contested amount among scientists. The most common number referenced appears to be around 1000 particles. (Reference 2) (Reference 3)
This number is derived from a previous viral study which compared viral dose level and infection rates. Studies of infectious dose levels of COVID-19, in particular, have not been conducted because of the ethical issue of purposely giving people a potentially deadly virus. (Reference 4)
Viral load is a commonly accepted concept with viruses. The more virus particles you breathe in, the more severe case of the virus you will contract. For example, if 1000 particles is the infectious dose level, and you breathe in 1000 particles, you will likely get a case of the virus. However, comparably, if you breathe in 100,000 particles, you will likely experience a more severe case of the virus. Similar to infectious dose, in-depth studies of viral load have not been performed on the population due to ethical concerns. (Reference 5)
The higher evaporation rate caused by lower humidity increases the density of the virus particles while longer periods of time indoors increase exposure time. This multiplication effect greatly increases our risk of contracting COVID-19 (or other viruses), especially in a more severe form.
Lower Ability to Shed Virus Particles
Once virus particles enter the respiratory system, they must adhere to ACE2 receptors of cells in order to infect the cell. In virus prevention, the goal is to keep virus particles from adhering to those receptors. Without that connection, the virus cannot infect the individual.
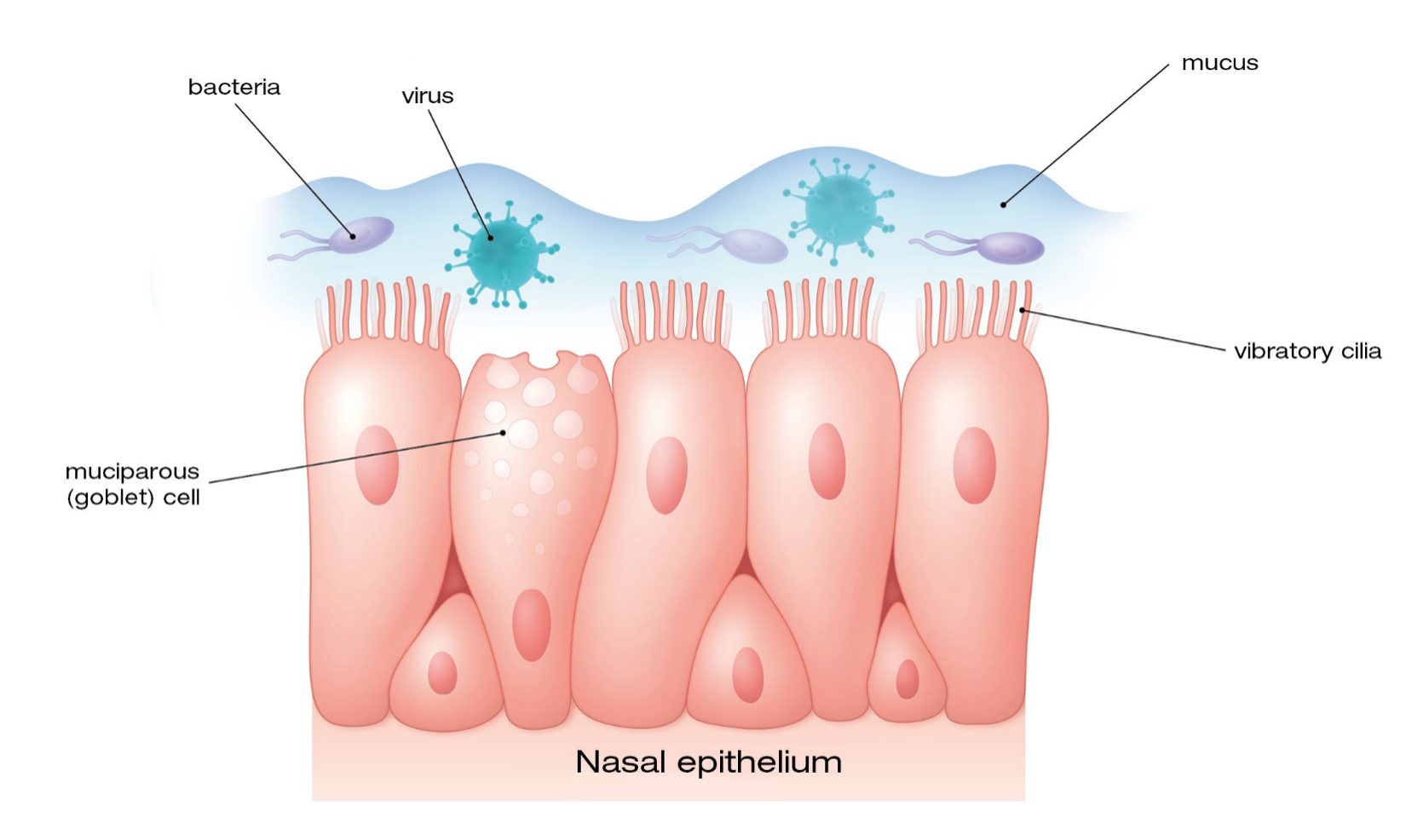
Our body has natural defenses against absorption of foreign particles within our respiratory system. The first is the cilia, which are small hairs that line the breathing passages. “Cilia wave in an upward direction and swipe up towards the throat any nasty material that gets stuck such as dust particles, bacteria or viruses.” (Reference 6) When humidity is lower, the cilia become less flexible and their sweeping action decreases. This decrease makes us more susceptible to virus contraction. Smokers and vapors, who already experience damaged cilia, are at a higher risk of viral contraction. (Reference 7)
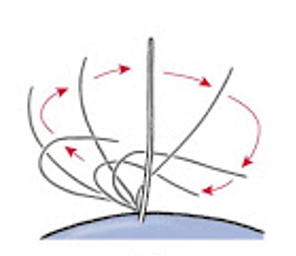
Cilia Movement BIOLOJOY: THE CELL
The second defense, working in coordination with the cilia, is the surface mucous liner of the mucous membrane inside of our breathing passages. The mucous, itself, acts as a barrier. With higher humidity levels, the mucous barrier is thickened. When humidity levels fall in the winter months, the mucous barrier can be significantly thinned, thus lowering our natural defenses, and making us more vulnerable.
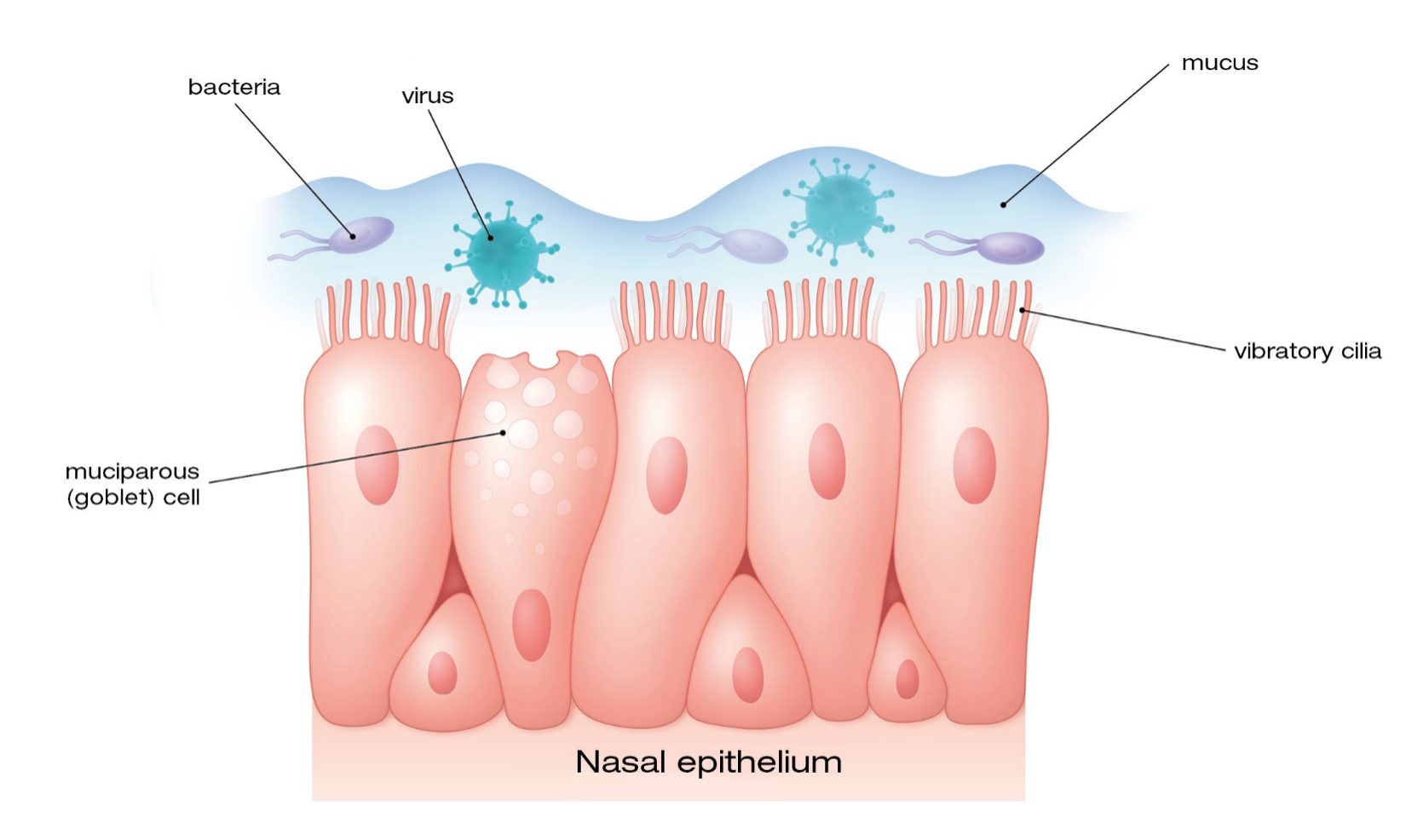
The nasal mucosa – Fitonasal 2Act
HVAC and Humidity
Viruses that thrive in high humidity levels are not nearly as concerning as those which thrive on the lower humidity end. Dehumidification is a common byproduct of most cooling processes, and typically leaves our indoor environments below the 60% RH level well below risk levels for high humidity viruses. While our buildings dehumidify, our buildings are not naturally protected from low humidity levels.
It is rather uncommon for most building types to implement humidification systems, even though there are many options of humidification systems in the market. In reality, the significant costs for humidification installation and the ongoing operation and maintenance of these systems are typically enough to deter their installation. The common process of bringing in colder outdoor air to provide fresh air within a building ends up drying out the air as the air warms. Outdoor air at 35 degrees and 95% RH will drop to about 25% RH when it is warmed up to 70 degrees within the HVAC system. This process leads to a constant drying out of our indoor air during the winter.
The process to overcome lower humidity levels by adding humidification systems is costly due to the process of humidification. Large volumes of water are required, and a phase change must occur to push the water from a liquid to a gas state. The amount of energy required to boil the water must be inserted into the process in some fashion to motivate the phase change. Additionally, any minerals or other items in the water can calcify within the system, or show up as dust within the space, unless the particles are removed from the water before the humidifier. As a result, it is currently uncommon to add humidification to a system unless it is necessary for specialty reasons such as paper processing and data centers, or where higher humidity can protect individuals at higher viral risk. An example of such is within hospitals. For this reason, the industry may see a slight increase in humidification installations within senior centers and nursing homes to help mitigate viral risk.
Clearly, humidity plays a direct role in the transmissibility of viruses including COVID-19. In colder winter months when humidity levels drop, a natural increase in viral transmission will likely continue to occur. Humidification systems can help to prevent the spread of viruses, but at an increased cost to the owner and building efficiency. Therefore, it is important for building design to continue to weigh the benefits of humidification versus the costs, as the world continues to battle new viral risks.
Engineering Tomorrow
At Allen + Shariff, we believe in providing innovative and efficient MEP engineering solutions to our clients. Contact us for more information on our ongoing blog series, to participate in a registered AIA seminar, or learn more about how you can partner with our team.
Contact Dave Van der Vossen at 910-218-3856 for details.
COVID-19 White Paper Series

COVID White Paper Series-06
 David Van der Vossen PE
David Van der Vossen PE
Senior VP of Engineering
LEED AP BD+C, CGD
As we continue our series on COVID-19 and preventable actions that we can put in place via building systems, let us take a deeper dive into the effect of humidity on transmission rates.
Hindsight is 20/20. Going into the winter, many experts predicted that we would see a significant uptick in COVID-19 cases. What did they know? Based on experience with other viruses such as the yearly flu, scientists knew that the combination of lower humidity and typical population patterns would most likely lead to an increase. Below is data from Johns Hopkins University that shows how this prediction played out between November 2020 and February 2021. As humidity levels decreased, COVID-19 cases did indeed grow.
ASHRAE has long noted the indirect health effects of humidity based on humidity’s effect on viruses, bacteria, and other pathogens. Below is a chart demonstrating the optimal safe zone between 40-60% RH (relative humidity).
Looking specifically at viruses; what is happening relative to lower humidity in the winter months? Three concepts come into play which play a role in the increase in transmission rates: higher evaporation rates, increased time indoors, and lower ability to shed virus particles.
Increasing Evaporation Rates
As virus particles are exhaled, they are incased in water and mucus. If the water and mucus evaporate before the droplet encounters a surface, then the virus particle will remain airborne. This allows the particle to spread easily throughout the space as people then breathe them in.
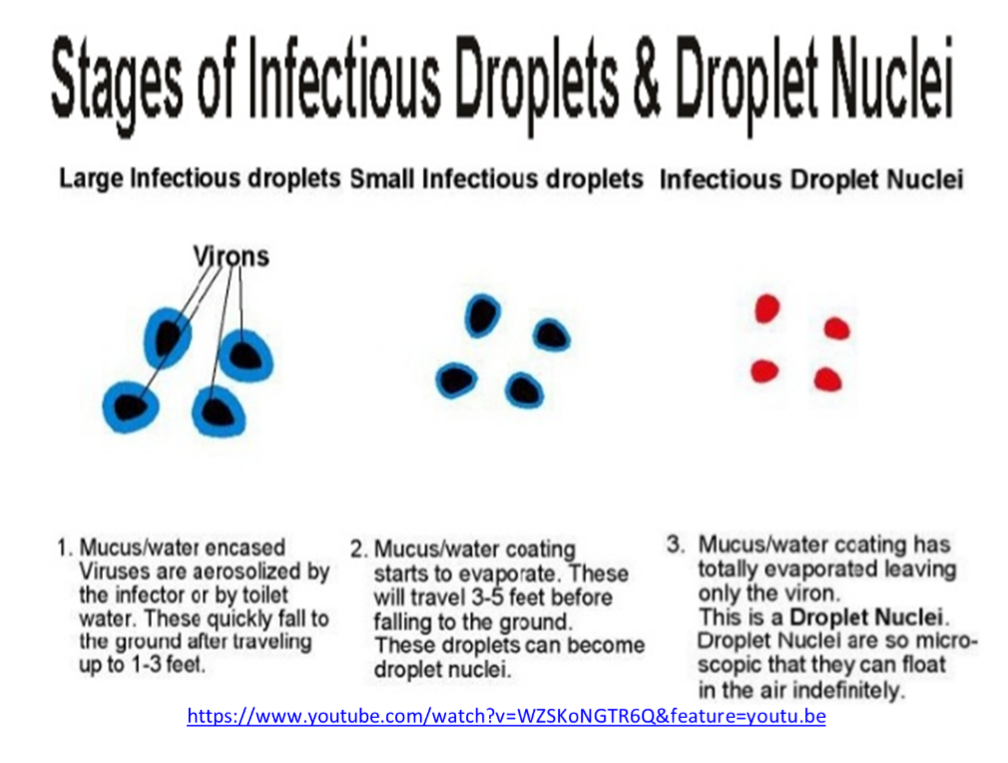
When humidity levels decrease, the number of virus particles that stay airborne rather than landing on a surface increase. During a 35-degree winter day, the indoor humidity of most homes and buildings will drop below 25% RH when no supplemental humidification system is present. This lower humidity significantly increases the number of droplets that evaporate and become aerosols. Thus, an increase in airborne concentration will increase the likelihood of people within the space breathing the virus in.
Time Indoors
In terms of aerosol transmission of viruses, exposure time and the aerosol concentration in a space are both significant players. The density of the virus particles in the air determines how many particles at any given time are ingested. How long someone stays within that environment also increases particle ingestion. Essentially, our exposure is equal to the rate of intake times the length of exposure. During the cold winter months, individuals inherently spend more time indoors, extending exposure time, and thus increasing transmission risk.
Exposure Risk
Breathing in a couple particles of COVID-19 will not give you the virus. To become infected, an individual needs to breathe in what is called an “infectious dose” level. The infectious dose level is a very contested amount among scientists. The most common number referenced appears to be around 1000 particles. (Reference 2) (Reference 3)
This number is derived from a previous viral study which compared viral dose level and infection rates. Studies of infectious dose levels of COVID-19, in particular, have not been conducted because of the ethical issue of purposely giving people a potentially deadly virus. (Reference 4)
Viral load is a commonly accepted concept with viruses. The more virus particles you breathe in, the more severe case of the virus you will contract. For example, if 1000 particles is the infectious dose level, and you breathe in 1000 particles, you will likely get a case of the virus. However, comparably, if you breathe in 100,000 particles, you will likely experience a more severe case of the virus. Similar to infectious dose, in-depth studies of viral load have not been performed on the population due to ethical concerns. (Reference 5)
The higher evaporation rate caused by lower humidity increases the density of the virus particles while longer periods of time indoors increase exposure time. This multiplication effect greatly increases our risk of contracting COVID-19 (or other viruses), especially in a more severe form.
Lower Ability to Shed Virus Particles
Once virus particles enter the respiratory system, they must adhere to ACE2 receptors of cells in order to infect the cell. In virus prevention, the goal is to keep virus particles from adhering to those receptors. Without that connection, the virus cannot infect the individual.
Our body has natural defenses against absorption of foreign particles within our respiratory system. The first is the cilia, which are small hairs that line the breathing passages. “Cilia wave in an upward direction and swipe up towards the throat any nasty material that gets stuck such as dust particles, bacteria or viruses.” (Reference 6) When humidity is lower, the cilia become less flexible and their sweeping action decreases. This decrease makes us more susceptible to virus contraction. Smokers and vapors, who already experience damaged cilia, are at a higher risk of viral contraction. (Reference 7)
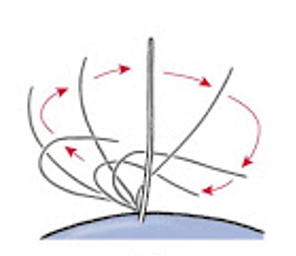
Cilia Movement BIOLOJOY: THE CELL
The second defense, working in coordination with the cilia, is the surface mucous liner of the mucous membrane inside of our breathing passages. The mucous, itself, acts as a barrier. With higher humidity levels, the mucous barrier is thickened. When humidity levels fall in the winter months, the mucous barrier can be significantly thinned, thus lowering our natural defenses, and making us more vulnerable.
The nasal mucosa – Fitonasal 2Act
HVAC and Humidity
Viruses that thrive in high humidity levels are not nearly as concerning as those which thrive on the lower humidity end. Dehumidification is a common byproduct of most cooling processes, and typically leaves our indoor environments below the 60% RH level well below risk levels for high humidity viruses. While our buildings dehumidify, our buildings are not naturally protected from low humidity levels.
It is rather uncommon for most building types to implement humidification systems, even though there are many options of humidification systems in the market. In reality, the significant costs for humidification installation and the ongoing operation and maintenance of these systems are typically enough to deter their installation. The common process of bringing in colder outdoor air to provide fresh air within a building ends up drying out the air as the air warms. Outdoor air at 35 degrees and 95% RH will drop to about 25% RH when it is warmed up to 70 degrees within the HVAC system. This process leads to a constant drying out of our indoor air during the winter.
The process to overcome lower humidity levels by adding humidification systems is costly due to the process of humidification. Large volumes of water are required, and a phase change must occur to push the water from a liquid to a gas state. The amount of energy required to boil the water must be inserted into the process in some fashion to motivate the phase change. Additionally, any minerals or other items in the water can calcify within the system, or show up as dust within the space, unless the particles are removed from the water before the humidifier. As a result, it is currently uncommon to add humidification to a system unless it is necessary for specialty reasons such as paper processing and data centers, or where higher humidity can protect individuals at higher viral risk. An example of such is within hospitals. For this reason, the industry may see a slight increase in humidification installations within senior centers and nursing homes to help mitigate viral risk.
Clearly, humidity plays a direct role in the transmissibility of viruses including COVID-19. In colder winter months when humidity levels drop, a natural increase in viral transmission will likely continue to occur. Humidification systems can help to prevent the spread of viruses, but at an increased cost to the owner and building efficiency. Therefore, it is important for building design to continue to weigh the benefits of humidification versus the costs, as the world continues to battle new viral risks.
Engineering Tomorrow
At Allen + Shariff, we believe in providing innovative and efficient MEP engineering solutions to our clients. Contact us for more information on our ongoing blog series, to participate in a registered AIA seminar, or learn more about how you can partner with our team.
Contact Dave Van der Vossen at 910-218-3856 for details.