COVID White Paper Series-07
 David Van der Vossen PE
David Van der Vossen PE
Senior VP of Engineering
LEED AP BD+C, CGD
As we continue our series on controlling air borne viruses, including COVID-19, we look at controlling the contaminant path. Two scenarios should be examined when discussing contaminant path. There are situations when we know who the virus carrier is; or we know who requires protection. The other scenario arises when we do not know the virus carrier and must protect all of the occupants.
Clean and Dirty Zones
There are many building environments where either the virus carrier is known, or we know the specific occupants requiring protection from potential carriers. Some of these environments may include:
- Staff and visitors at COVID ICU rooms
- Nurses and doctors at nurses’ stations
- Staff at reception areas
- Elderly at nursing homes
These occurrences are more straightforward to address in MEP design because we know who and where to provide protection. We can simplify the HVAC design approach to providing clean air in the clean zone and exhausting or returning air from the dirty zone. This exhausting of the virus is the same concept as exhausting a bathroom or kitchen. The closer the HVAC system is to the contaminant source; the greater number of contaminants it can capture. In hospital rooms and doctors’ offices, the preferred design approach is to provide air behind the doctor or staff. The air then sweeps across the patient area and returns or exhausts down low behind the patient.
https://www.slideshare.net/sharrygajuryalnepal/isolation-facility
Nursing stations, unlike patient rooms, are typically open to the adjacent corridors to facilitate nursing duties throughout the day. During the early stages of the pandemic, several hospitals framed up plastic walls to enclose these nursing stations. This served a dual purpose. First, it limited the direct path of transmission for droplets. Second, it allowed the hospital to provide the supply air grilles in the nursing station and move the return air grilles to the corridor areas. By doing so, a clean zone within the nurses’ station is provided. The potentially contaminated air is pushed towards the hallway. The nurses’ station, therefore, became an “area of refuge” from virus contamination.


ZipWall COVID Containment | ZipWall Barriers in Healthcare | zipwall.com
In reception areas, similar measures can be implemented in a more permanent solution. Whether glass partitions are implemented or not, it will become more commonplace in HVAC design to provide the clean supply air within the staff area while providing returns out in the visitor area. This will sweep clean air past the staff and limit contaminants reaching the staff via visitors. This design approach of providing clean and dirty zones is standard. Supply is provided in one area with exhaust/return in another. This approach can be simple and easy. Or the design can be taken to more extreme measures by incorporating ante rooms and other higher end measures depending on the severity of the virus risk.
Making Everywhere a Clean Zone
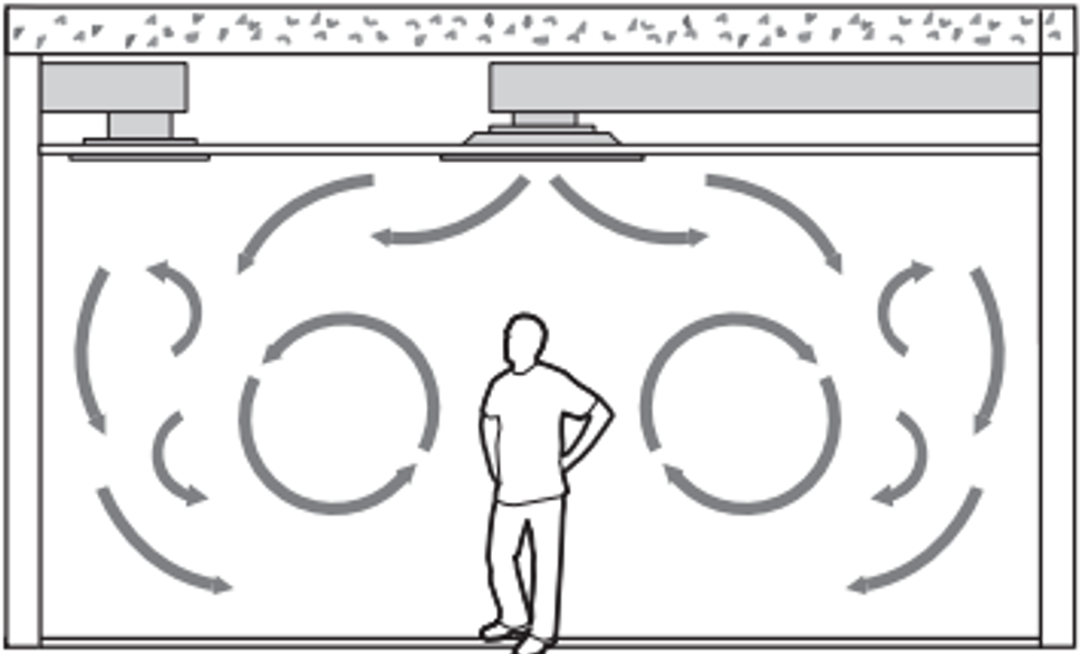
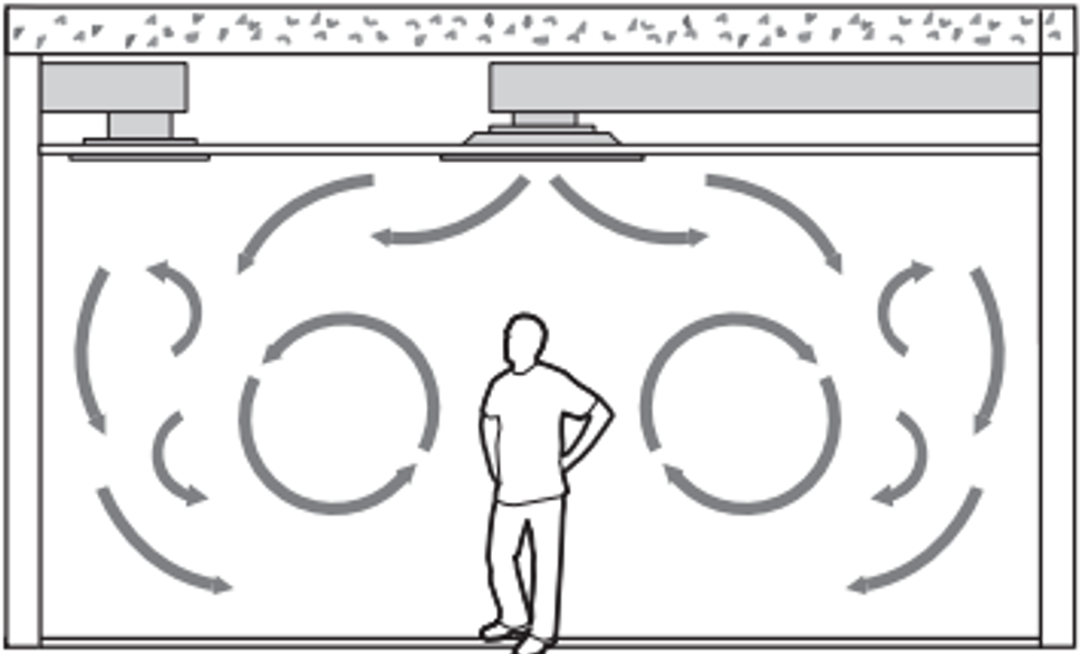
The second category of contaminant path to address is when we do not recognize the virus carrier and therefore, must protect all of the occupants. Standard HVAC design practices in commercial buildings provide the supply and return grilles at the ceiling, thus, churning the air to achieve effective mixing across the occupied space.
https://www.simscale.com/wp-content/uploads/2017/12/displacement-ventilation-vs-mixing.png
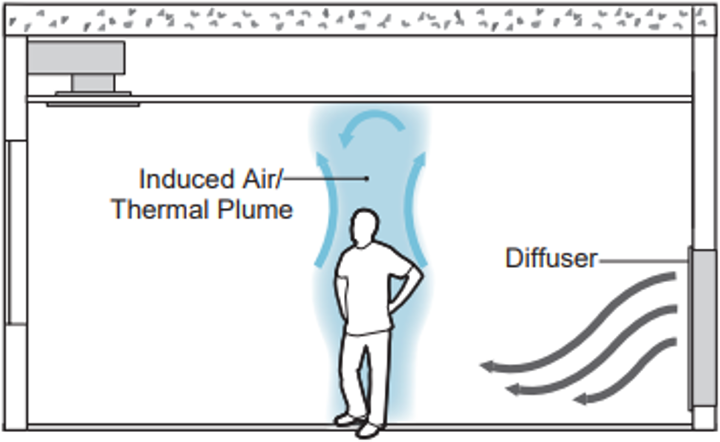
With this mixing of air, contaminant control must take a different approach. This approach entails slowing down the air, supplying the air low, and then returning the air high. This method reduces mixing and carries the contaminants towards the ceiling, away from the breathing zone of other occupants. This design method is effective when cooling buildings. Two methodologies are especially effective when trying to cool a space. The first method is to use low mounted displacement diffusers throughout the space. These diffusers are larger and designed to slowly spill the air out of the diffuser. The dispensed air then creeps across the floor. As the air encounters heating sources such as people, computers, etc., the air is heated up and an induced thermal plume will occur around the heating source. As this air flows upward around the person, the movement will entrain the contaminants from the breathing zone and carry them toward the ceiling or “hot zone”.
https://www.simscale.com/wp-content/uploads/2017/12/displacement-ventilation-vs-mixing.png
This distribution approach only works, however, for “cooling-only zones.” Cooling-only zones are typically a building’s interior spaces that do not have exterior heating requirements. Or they may be in buildings that are geographically farther south, and thus, do not typically require heating to be run. If heating is integrated with this system, the warm supply air will head straight towards the ceiling and not heat the occupied space. Supplemental radiant heating could be added to these spaces in various ways. However, whenever the space is in heating mode, no cold air would be supplied at the floor, and thus no induced thermal plumes would exist. The contaminant path is, therefore, not controlled in heating mode.
The second methodology of air distribution is the utilization of an underfloor distribution system. However, some changes should be addressed compared to how underfloor systems have historically been designed. Historically, most underfloor systems are designed with greater air velocities, creating a churning of the air that is too great to control the contaminant path. To offset this air churning, larger quantities of grilles and physically larger grilles are required to slow the air down. The goal of the air distribution is for the airflow to be laminar before it reaches the breathing zone of the occupant. In this way, we can once again create an induced thermal plume and carry contaminated air towards the ceiling.

This approach will also work better than the previous methodology during the heating cycle. With enough evenly spaced grilles, a consistent flow of air from the floor toward the ceiling can be created to carry the contaminants from the breathing zone towards the ceiling even during heating modes.
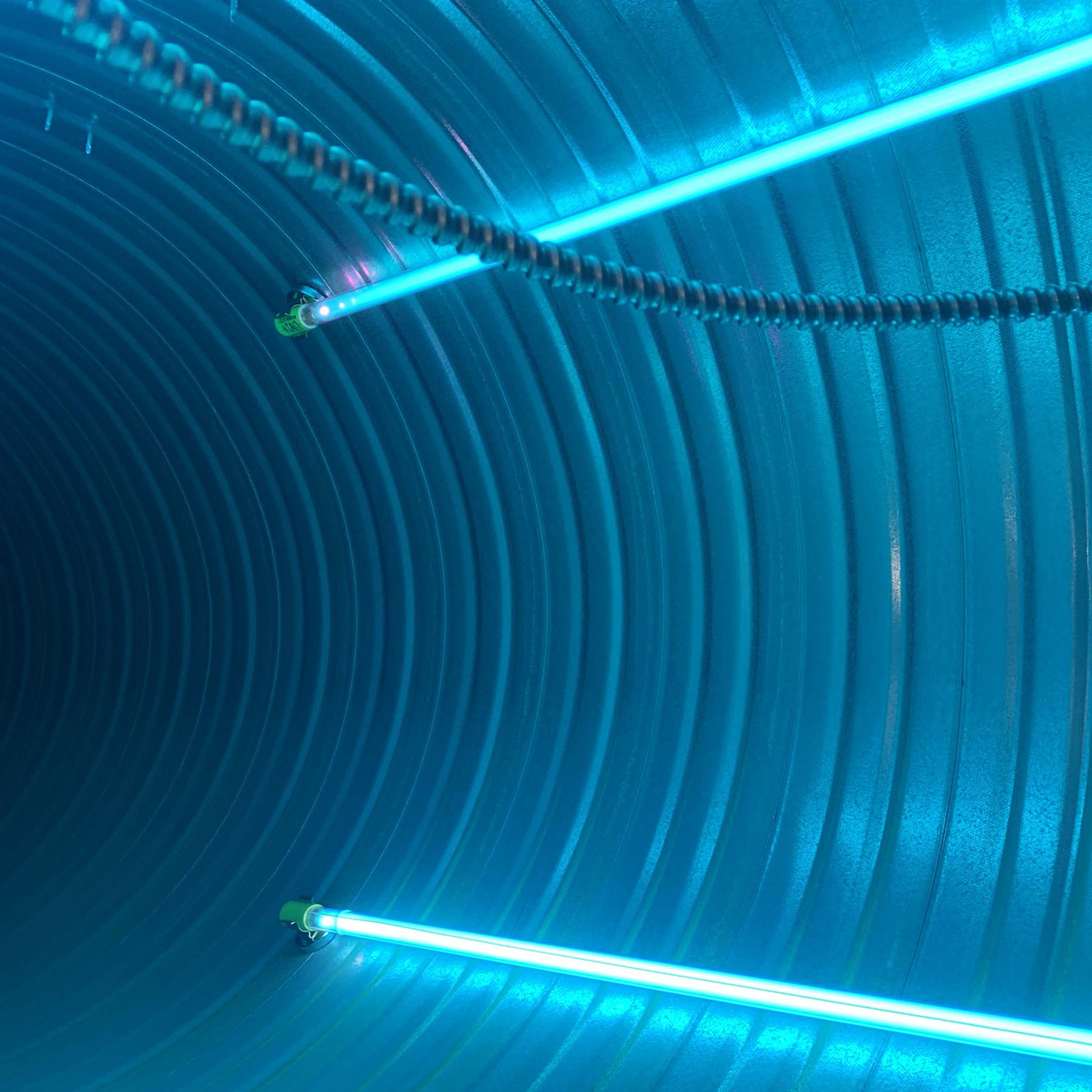
From a design perspective, both HVAC solutions require more space and in-turn, more money, to incorporate them into a building. The standard design of above ceiling supply and returns is significantly cheaper, thus making it the go-to common solution. For many existing buildings, it may not be practical to incorporate either of the two air distribution methodologies. In these cases, implementing other pathogen control strategies such as higher filtration and UVC will be more cost-effective approaches.
Engineering Tomorrow
At Allen + Shariff, we believe in providing innovative and efficient MEP engineering solutions to our clients. Contact us for more information on our ongoing blog series, to participate in a registered AIA seminar, or learn more about how you can partner with our team.
Contact Dave Van der Vossen at 910-218-3856 for details.
COVID-19 White Paper Series

COVID White Paper Series-07
 David Van der Vossen PE
David Van der Vossen PE
Senior VP of Engineering
LEED AP BD+C, CGD
As we continue our series on controlling air borne viruses, including COVID-19, we look at controlling the contaminant path. Two scenarios should be examined when discussing contaminant path. There are situations when we know who the virus carrier is; or we know who requires protection. The other scenario arises when we do not know the virus carrier and must protect all of the occupants.
Clean and Dirty Zones
There are many building environments where either the virus carrier is known, or we know the specific occupants requiring protection from potential carriers. Some of these environments may include:
- Staff and visitors at COVID ICU rooms
- Nurses and doctors at nurses’ stations
- Staff at reception areas
- Elderly at nursing homes
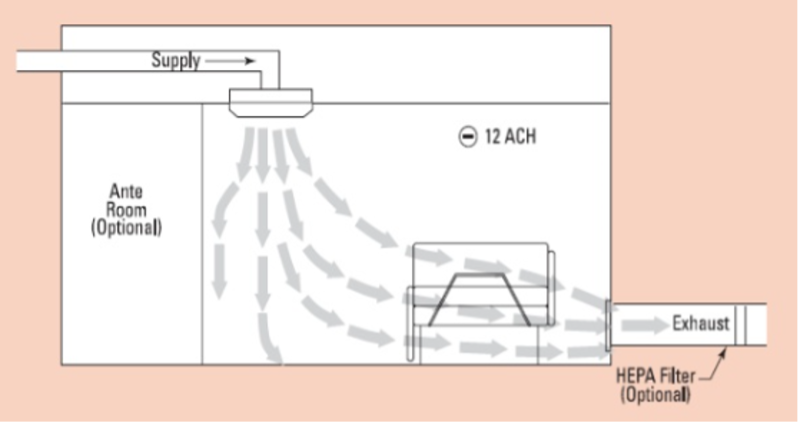
These occurrences are more straightforward to address in MEP design because we know who and where to provide protection. We can simplify the HVAC design approach to providing clean air in the clean zone and exhausting or returning air from the dirty zone. This exhausting of the virus is the same concept as exhausting a bathroom or kitchen. The closer the HVAC system is to the contaminant source; the greater number of contaminants it can capture. In hospital rooms and doctors’ offices, the preferred design approach is to provide air behind the doctor or staff. The air then sweeps across the patient area and returns or exhausts down low behind the patient.
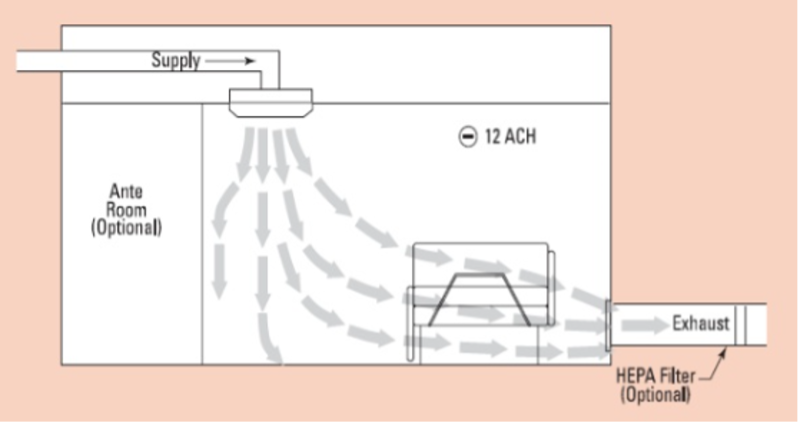
https://www.slideshare.net/sharrygajuryalnepal/isolation-facility
Nursing stations, unlike patient rooms, are typically open to the adjacent corridors to facilitate nursing duties throughout the day. During the early stages of the pandemic, several hospitals framed up plastic walls to enclose these nursing stations. This served a dual purpose. First, it limited the direct path of transmission for droplets. Second, it allowed the hospital to provide the supply air grilles in the nursing station and move the return air grilles to the corridor areas. By doing so, a clean zone within the nurses’ station is provided. The potentially contaminated air is pushed towards the hallway. The nurses’ station, therefore, became an “area of refuge” from virus contamination.


ZipWall COVID Containment | ZipWall Barriers in Healthcare | zipwall.com
In reception areas, similar measures can be implemented in a more permanent solution. Whether glass partitions are implemented or not, it will become more commonplace in HVAC design to provide the clean supply air within the staff area while providing returns out in the visitor area. This will sweep clean air past the staff and limit contaminants reaching the staff via visitors. This design approach of providing clean and dirty zones is standard. Supply is provided in one area with exhaust/return in another. This approach can be simple and easy. Or the design can be taken to more extreme measures by incorporating ante rooms and other higher end measures depending on the severity of the virus risk.
Making Everywhere a Clean Zone
The second category of contaminant path to address is when we do not recognize the virus carrier and therefore, must protect all of the occupants. Standard HVAC design practices in commercial buildings provide the supply and return grilles at the ceiling, thus, churning the air to achieve effective mixing across the occupied space.
https://www.simscale.com/wp-content/uploads/2017/12/displacement-ventilation-vs-mixing.png
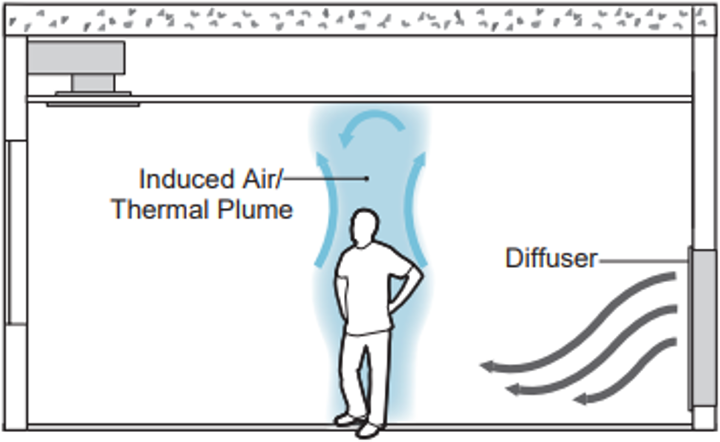
With this mixing of air, contaminant control must take a different approach. This approach entails slowing down the air, supplying the air low, and then returning the air high. This method reduces mixing and carries the contaminants towards the ceiling, away from the breathing zone of other occupants. This design method is effective when cooling buildings. Two methodologies are especially effective when trying to cool a space. The first method is to use low mounted displacement diffusers throughout the space. These diffusers are larger and designed to slowly spill the air out of the diffuser. The dispensed air then creeps across the floor. As the air encounters heating sources such as people, computers, etc., the air is heated up and an induced thermal plume will occur around the heating source. As this air flows upward around the person, the movement will entrain the contaminants from the breathing zone and carry them toward the ceiling or “hot zone”.
https://www.simscale.com/wp-content/uploads/2017/12/displacement-ventilation-vs-mixing.png
This distribution approach only works, however, for “cooling-only zones.” Cooling-only zones are typically a building’s interior spaces that do not have exterior heating requirements. Or they may be in buildings that are geographically farther south, and thus, do not typically require heating to be run. If heating is integrated with this system, the warm supply air will head straight towards the ceiling and not heat the occupied space. Supplemental radiant heating could be added to these spaces in various ways. However, whenever the space is in heating mode, no cold air would be supplied at the floor, and thus no induced thermal plumes would exist. The contaminant path is, therefore, not controlled in heating mode.
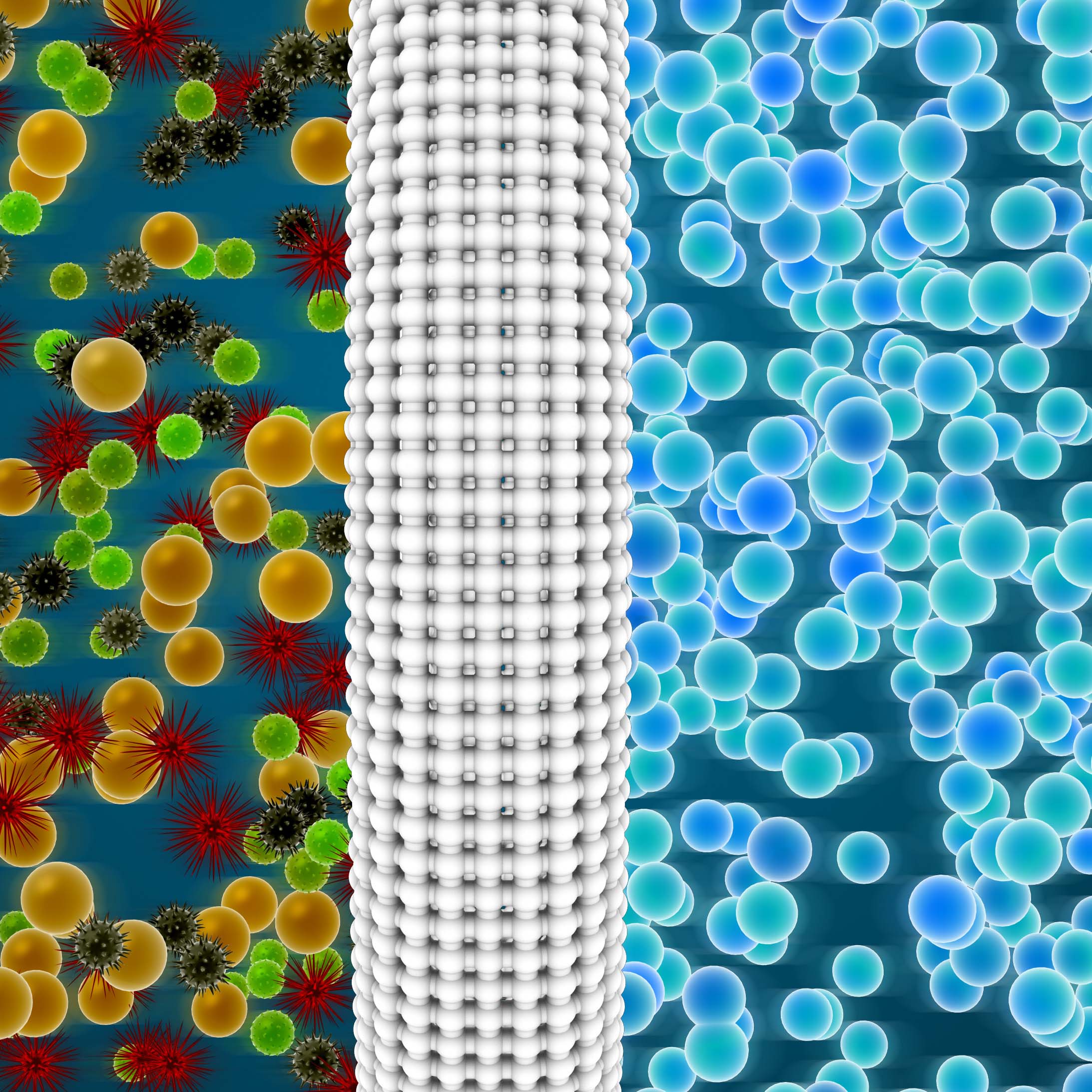
The second methodology of air distribution is the utilization of an underfloor distribution system. However, some changes should be addressed compared to how underfloor systems have historically been designed. Historically, most underfloor systems are designed with greater air velocities, creating a churning of the air that is too great to control the contaminant path. To offset this air churning, larger quantities of grilles and physically larger grilles are required to slow the air down. The goal of the air distribution is for the airflow to be laminar before it reaches the breathing zone of the occupant. In this way, we can once again create an induced thermal plume and carry contaminated air towards the ceiling.

This approach will also work better than the previous methodology during the heating cycle. With enough evenly spaced grilles, a consistent flow of air from the floor toward the ceiling can be created to carry the contaminants from the breathing zone towards the ceiling even during heating modes.
From a design perspective, both HVAC solutions require more space and in-turn, more money, to incorporate them into a building. The standard design of above ceiling supply and returns is significantly cheaper, thus making it the go-to common solution. For many existing buildings, it may not be practical to incorporate either of the two air distribution methodologies. In these cases, implementing other pathogen control strategies such as higher filtration and UVC will be more cost-effective approaches.
Engineering Tomorrow
At Allen + Shariff, we believe in providing innovative and efficient MEP engineering solutions to our clients. Contact us for more information on our ongoing blog series, to participate in a registered AIA seminar, or learn more about how you can partner with our team.
Contact Dave Van der Vossen at 910-218-3856 for details.