By David Van der Vossen, PE
By David Van der Vossen, PE
Senior VP of Engineering
LEED AP BD+C, CGD
The COVID-19 Pandemic has brought a renewed focus on how to protect workers in the built environment. As more states see a decline in COVID cases and workers return to the office, businesses need to implement the best systems to keep their workers safe and healthy.
This is the first in our blog series that will review how the virus is transmitted and how we can reduce transmission rates through MEP system changes. Over the next several weeks, we invite you to join us as we take a deeper dive into the following topics:
1 – Why HVAC plays a significant role in reducing transmission rates
2 – The First Step: Increasing Ventilation
3 – Filtration: Is it here to stay?
4 – UVC: Why this is the standard recommended by ASHRAE and CDC
5 – Needlepoint bi-polar ionization: Up and coming technology
6 – How humidity comes into play
7 – Controlling the contaminant path
8 – Circadian lighting: What does the Science Say?
9 – Likely HVAC Design Changes Post COVID-19
Transmission Methods
COVID-19 is transmitted in three different ways:
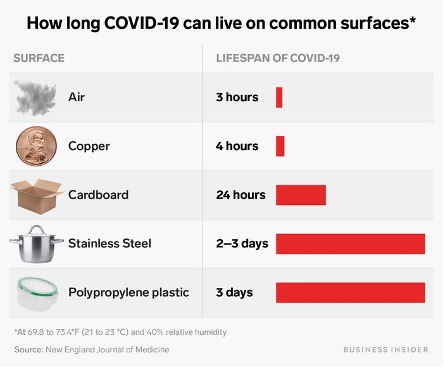
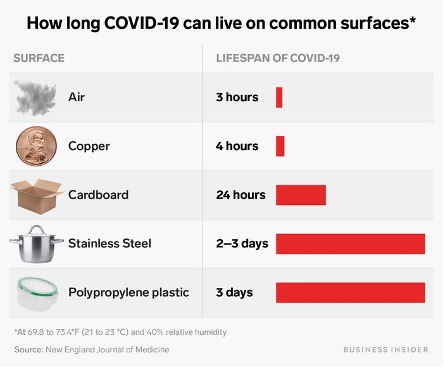
Fomite
This is direct surface transmission. The common analogy is a carrier coughs on their hand, touches a doorknob, which in turn is touched by the next person who then touches their face. On 5/22/2020 the CDC first stated this “isn’t thought to be the main way the virus spreads.” (Reference 1—Centers for Disease Control)
If your primary mitigation strategy revolves around cleaning and disinfecting, then you are missing the main causes of COVID-19.
Droplets/Close Contact
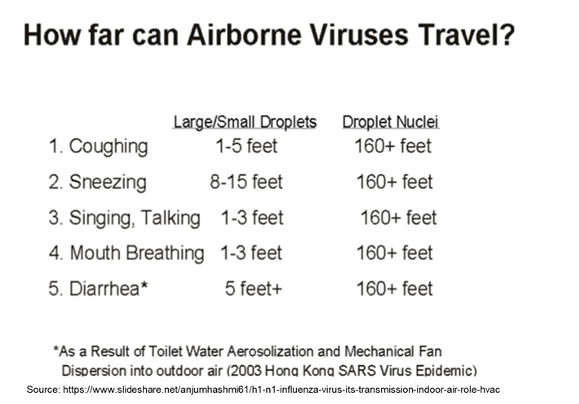
These are larger droplets that are being exhaled (cough, sneeze, talking, etc.) and coming in direct contact with the nose, eyes, mouth or ears of someone in close proximity to the carrier. This was originally thought to be one of the main transmission methods that can be mitigated using masks and screens.
Aerosols: Virons, Droplet Nuclei & Micro Droplets
While it comes with many names, this is the other common transmission method, but was largely under recognized by the WHO & CDC until an open letter to the WHO from 238 scientists and researchers pushed the issue. (Reference 2—Oxford Academic)
Interestingly the CDC alludes to micro droplet transmission in several earlier case studies. (Reference 3—Centers for Disease Control)
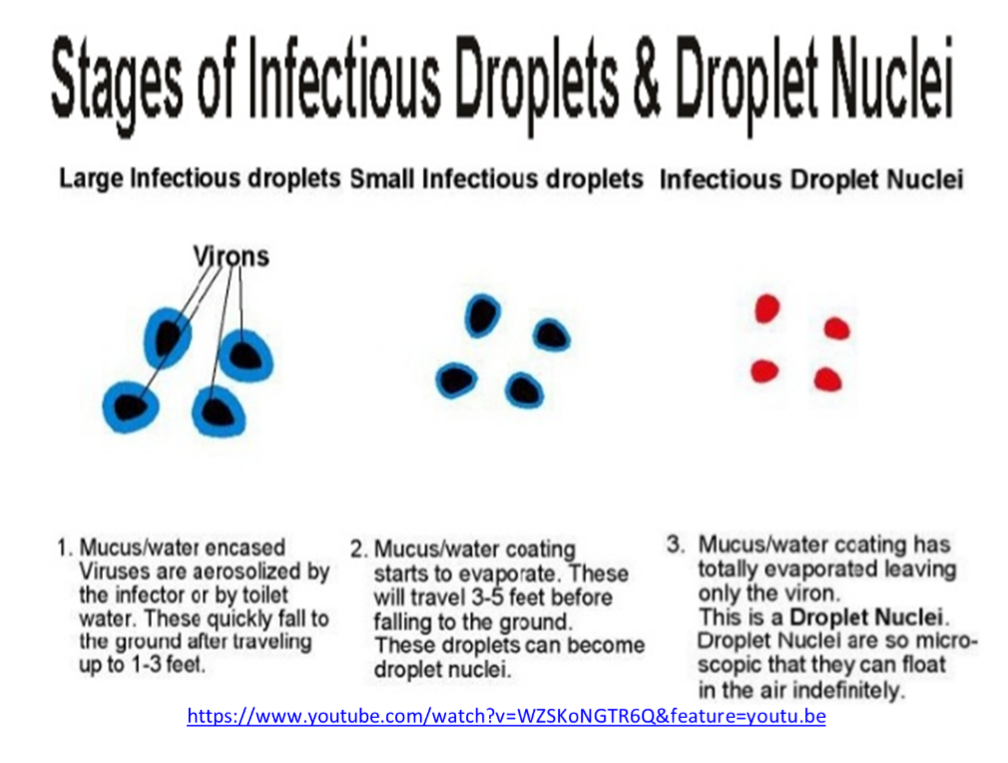
As virus particles are exhaled, they are incased in water and mucus. If the water and mucus evaporate before the droplet comes in contact with a surface, then the virus particle will remain airborne and spread throughout the space. Other people in the space can then breath in these particles.
Infectious Dose Level & Viral Load
If you breath in a couple particles of COVID-19 you are not going to catch the virus. You need to breath in what is called an “infectious dose” level. The infectious dose level is a very contested amount, but the most common numbers referenced appear to be around 1000 particles. (Reference 4—Centers For Disease Control)
This is based on analysis of looking at other viruses and comparing their infectious dose level and infection rates to that of COVID-19. Studies of infectious dose level of COVID-19 have not been conducted because of the ethical issue of purposely giving people a potentially deadly virus. (Reference 5—Science Media Culture Blog)
The average person carrier sitting at their desk expels 33 virus particles per minute. As you increase activity level, the amount of virus particles expelled increases. When one coughs, it can be a couple hundred thousand virus particles and as you sneeze, it can be a couple million virus particles. (Reference 6—Matthew J. Evans, MIT, Department of Physics)
The amount that stay airborne versus the amount that quickly settle nearby on adjacent surfaces can vary significantly.
Viral load is a commonly accepted concept with viruses. The more virus particles you breath in the more severe case of the virus you will get. For example, if 1000 particles is the infectious dose level and you breath in 1000 particles, then you will likely get a minor case of the virus, but if you breathe in 100,000 particles, then you will likely come down with a much more severe case of the virus. Similar to infectious dose, in depth studies of Viral load have not been performed on people because of ethical concerns. (Reference 7—New Scientist)
When we look at airborne or aerosol transmission of the virus, the length of the exposure and the density of the virus in a space are both significant players. The density of the virus particles in the space determines how many virus particles per any given time we are bringing into our body. The length of time in the environment effects the total intake of virus particles. Essentially, our exposure is equal to the rate of intake times the length of exposure.
Why HVAC Plays a Significant Role
With HVAC systems we can affect the density of the virus particles in a space, thereby extending the time before someone reaches an infectious dose level. Our goal with HVAC is to reduce the density of virus particles to the point where no one is exposed to an infectious dose level. Even if we are not able to eliminate everyone from reaching the infectious dose level, every step we take will reduce the number of occupants reaching the infectious dose level and will reduce everyone’s viral load (the number of particles absorbed) which will result in much less severe cases of the virus.
Our goal with HVAC systems is to reduce the number of virus particles contained within the space. The most common approaches include diluting, filtering, and deactivating the virus particles. We will go into more detail over the next several weeks on all these approaches.
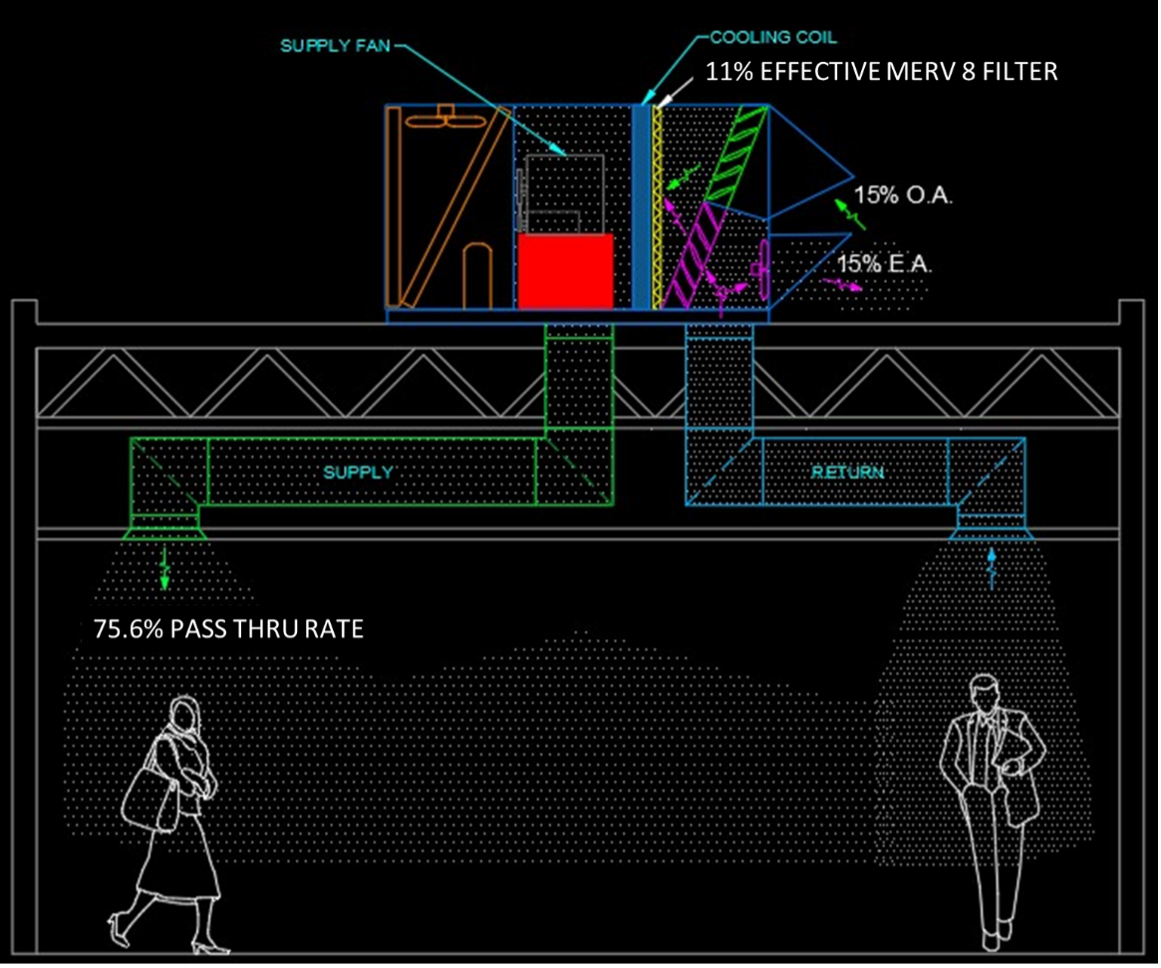
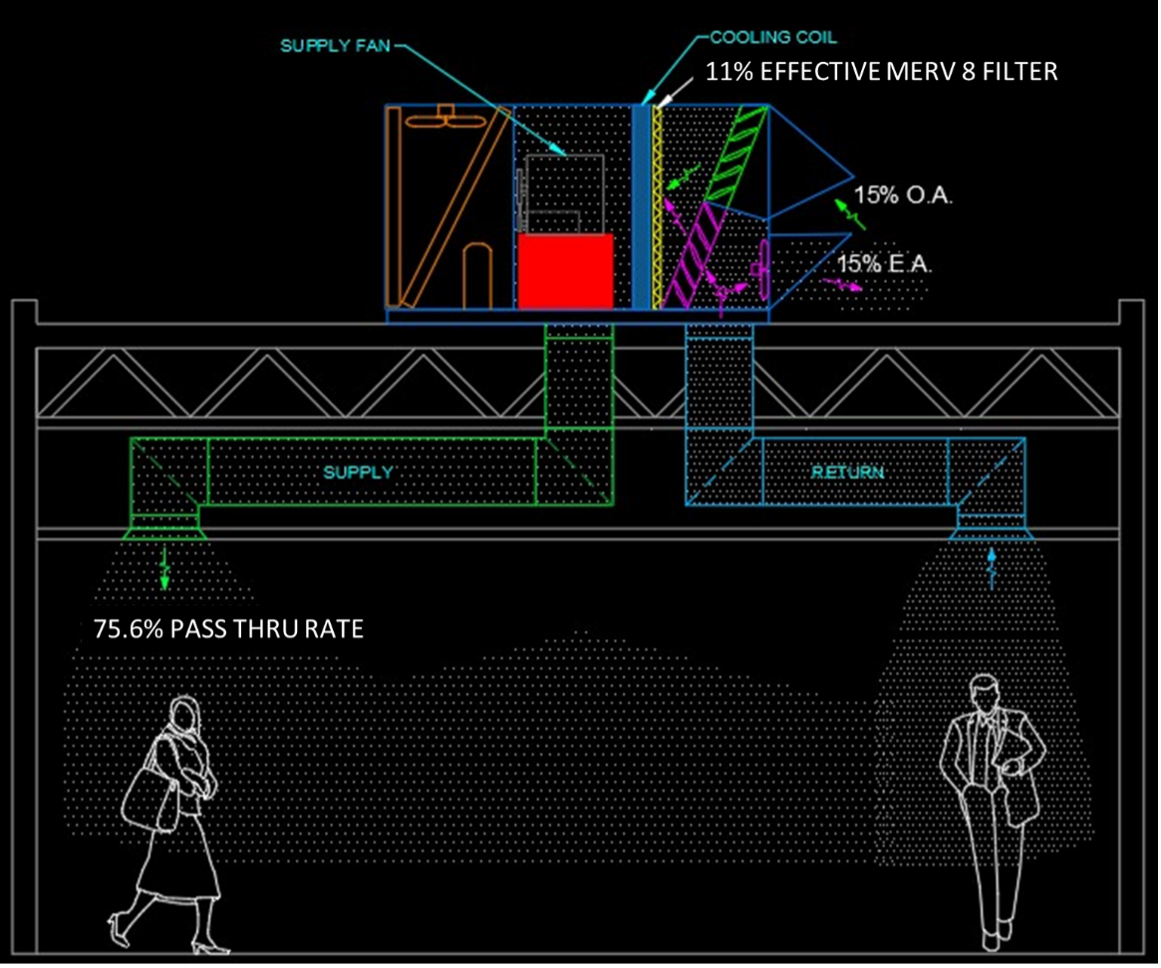
We will leave you with example project that we will use over the next several weeks to analyze the effectiveness of our approaches. In this space we have a rooftop unit which is delivering 15% outdoor air and is utilizing a standard MERV8 filter. We assume that our system capacity runs all the air through our space four to six times per hour. All of these are base norms are used in many applications and are a good starting point for our comparisons. As you will notice in the diagram below, we have a pass thru rate of 75.6%. This means the effectiveness of our system in removing virus particles from the space is 24.4%. Four to six times per hour the room volume passes thru our HVAC unit and each time it removes 24.4% of the virus particles. At the same time, if there is a carrier in the space, they are adding more virus particles to the air. Our goal is to increase our effectiveness and lower the pass thru rate with the approaches we will review in the coming weeks.
Engineering Tomorrow
At Allen + Shariff, we believe in providing innovative and efficient MEP engineering solutions to our clients. Contact us for more information on our ongoing blog series, to participate in a registered AIA seminar, or learn more about how you can partner with our team.
Contact Dave Van der Vossen at 910-218-3856 for details.

 By David Van der Vossen, PE
By David Van der Vossen, PE
Senior VP of Engineering
LEED AP BD+C, CGD
The COVID-19 Pandemic has brought a renewed focus on how to protect workers in the built environment. As more states see a decline in COVID cases and workers return to the office, businesses need to implement the best systems to keep their workers safe and healthy.
This is the first in our blog series that will review how the virus is transmitted and how we can reduce transmission rates through MEP system changes. Over the next several weeks, we invite you to join us as we take a deeper dive into the following topics:
1 – Why HVAC plays a significant role in reducing transmission rates
2 – The First Step: Increasing Ventilation
3 – Filtration: Is it here to stay?
4 – UVC: Why this is the standard recommended by ASHRAE and CDC
5 – Needlepoint bi-polar ionization: Up and coming technology
6 – How humidity comes into play
7 – Controlling the contaminant path
8 – Circadian lighting: What does the Science Say?
9 – Likely HVAC Design Changes Post COVID-19
Transmission Methods
COVID-19 is transmitted in three different ways:
Fomite
This is direct surface transmission. The common analogy is a carrier coughs on their hand, touches a doorknob, which in turn is touched by the next person who then touches their face. On 5/22/2020 the CDC first stated this “isn’t thought to be the main way the virus spreads.” (Reference 1—Centers for Disease Control)
If your primary mitigation strategy revolves around cleaning and disinfecting, then you are missing the main causes of COVID-19.
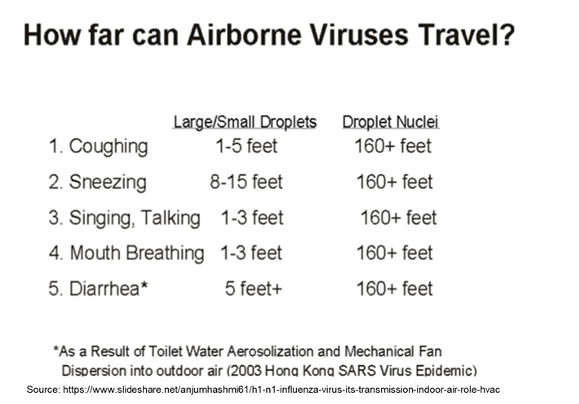
Droplets/Close Contact
These are larger droplets that are being exhaled (cough, sneeze, talking, etc.) and coming in direct contact with the nose, eyes, mouth or ears of someone in close proximity to the carrier. This was originally thought to be one of the main transmission methods that can be mitigated using masks and screens.
Aerosols: Virons, Droplet Nuclei & Micro Droplets
While it comes with many names, this is the other common transmission method, but was largely under recognized by the WHO & CDC until an open letter to the WHO from 238 scientists and researchers pushed the issue. (Reference 2—Oxford Academic)
Interestingly the CDC alludes to micro droplet transmission in several earlier case studies. (Reference 3—Centers for Disease Control)
As virus particles are exhaled, they are incased in water and mucus. If the water and mucus evaporate before the droplet comes in contact with a surface, then the virus particle will remain airborne and spread throughout the space. Other people in the space can then breath in these particles.
Infectious Dose Level & Viral Load
If you breath in a couple particles of COVID-19 you are not going to catch the virus. You need to breath in what is called an “infectious dose” level. The infectious dose level is a very contested amount, but the most common numbers referenced appear to be around 1000 particles. (Reference 4—Centers For Disease Control)
This is based on analysis of looking at other viruses and comparing their infectious dose level and infection rates to that of COVID-19. Studies of infectious dose level of COVID-19 have not been conducted because of the ethical issue of purposely giving people a potentially deadly virus. (Reference 5—Science Media Culture Blog)
The average person carrier sitting at their desk expels 33 virus particles per minute. As you increase activity level, the amount of virus particles expelled increases. When one coughs, it can be a couple hundred thousand virus particles and as you sneeze, it can be a couple million virus particles. (Reference 6—Matthew J. Evans, MIT, Department of Physics)
The amount that stay airborne versus the amount that quickly settle nearby on adjacent surfaces can vary significantly.
Viral load is a commonly accepted concept with viruses. The more virus particles you breath in the more severe case of the virus you will get. For example, if 1000 particles is the infectious dose level and you breath in 1000 particles, then you will likely get a minor case of the virus, but if you breathe in 100,000 particles, then you will likely come down with a much more severe case of the virus. Similar to infectious dose, in depth studies of Viral load have not been performed on people because of ethical concerns. (Reference 7—New Scientist)
When we look at airborne or aerosol transmission of the virus, the length of the exposure and the density of the virus in a space are both significant players. The density of the virus particles in the space determines how many virus particles per any given time we are bringing into our body. The length of time in the environment effects the total intake of virus particles. Essentially, our exposure is equal to the rate of intake times the length of exposure.
Why HVAC Plays a Significant Role
With HVAC systems we can affect the density of the virus particles in a space, thereby extending the time before someone reaches an infectious dose level. Our goal with HVAC is to reduce the density of virus particles to the point where no one is exposed to an infectious dose level. Even if we are not able to eliminate everyone from reaching the infectious dose level, every step we take will reduce the number of occupants reaching the infectious dose level and will reduce everyone’s viral load (the number of particles absorbed) which will result in much less severe cases of the virus.
Our goal with HVAC systems is to reduce the number of virus particles contained within the space. The most common approaches include diluting, filtering, and deactivating the virus particles. We will go into more detail over the next several weeks on all these approaches.
We will leave you with example project that we will use over the next several weeks to analyze the effectiveness of our approaches. In this space we have a rooftop unit which is delivering 15% outdoor air and is utilizing a standard MERV8 filter. We assume that our system capacity runs all the air through our space four to six times per hour. All of these are base norms are used in many applications and are a good starting point for our comparisons. As you will notice in the diagram below, we have a pass thru rate of 75.6%. This means the effectiveness of our system in removing virus particles from the space is 24.4%. Four to six times per hour the room volume passes thru our HVAC unit and each time it removes 24.4% of the virus particles. At the same time, if there is a carrier in the space, they are adding more virus particles to the air. Our goal is to increase our effectiveness and lower the pass thru rate with the approaches we will review in the coming weeks.
Engineering Tomorrow
At Allen + Shariff, we believe in providing innovative and efficient MEP engineering solutions to our clients. Contact us for more information on our ongoing blog series, to participate in a registered AIA seminar, or learn more about how you can partner with our team.
Contact Dave Van der Vossen at 910-218-3856 for details.